Invented by David W. Weir, Joseph M. Arsanious, Gabriel F. Brisson, Niels Smaby, Intuitive Surgical Operations Inc
In any surgical procedure, interruptions are inevitable. Whether it is due to power outages, equipment malfunctions, or even human error, these interruptions can disrupt the flow of the procedure and potentially lead to complications. Restoring instrument control input position/orientation technology addresses this issue by providing a solution that allows surgeons to pick up where they left off, without having to start the procedure from scratch.
One of the key factors driving the market for this technology is the increasing demand for minimally invasive surgeries. These procedures require precise control and maneuverability of surgical instruments, and any disruption in the control input position/orientation can have serious consequences. Restoring instrument control input position/orientation technology ensures that surgeons can maintain the desired position and orientation of the instruments, even after an interruption, thereby reducing the risk of complications and improving patient outcomes.
Another factor contributing to the growth of this market is the advancements in robotic surgery. Robotic surgical systems have become increasingly popular in recent years due to their ability to enhance surgical precision and control. However, these systems are not immune to interruptions. Restoring instrument control input position/orientation technology plays a crucial role in robotic surgeries by allowing the system to resume operations seamlessly, minimizing the impact of interruptions on the overall procedure.
Furthermore, the market for restoring instrument control input position/orientation technology is also driven by the increasing adoption of virtual reality (VR) and augmented reality (AR) in surgical procedures. These technologies provide surgeons with real-time visualization and guidance during operations, enhancing their ability to perform complex procedures. Restoring instrument control input position/orientation technology complements VR and AR by ensuring that the surgeon’s control input remains accurate and consistent, even in the event of interruptions.
In terms of geographical distribution, North America is expected to dominate the market for restoring instrument control input position/orientation technology. The region has a well-established healthcare infrastructure and a high adoption rate of advanced surgical technologies. Additionally, the presence of major market players and ongoing research and development activities further contribute to the growth of this market in North America.
Overall, the market for restoring instrument control input position/orientation during midprocedure restart is witnessing significant growth due to the increasing demand for minimally invasive surgeries, advancements in robotic surgery, and the adoption of VR and AR technologies. As the technology continues to evolve and improve, it is expected to become an integral part of surgical procedures, ensuring uninterrupted and precise control over surgical instruments.

The Intuitive Surgical Operations Inc invention works as follows
A robotic system consists of a robotic assembly consisting of a drive mechanism and sensor assembly. The controller is communicatively connected to the sensor assemblies. The controller contains at least one processor that is configured to execute a procedure. The method includes recording the position of the drive mechanisms to non-volatile memories during use of a robotic assembly, and receiving a demand to initiate a middle-procedure start-up of the robot assembly after a shutdown of the assembly in the middle of a procedure. The method further comprises determining if a position of a drive mechanism after a shutdown is within a tolerance relative to its pre-shutdown and stopping the use of the robotic system in response to that determination.

Background for Restoring instrument control input position/orientation during midprocedure restart
Minimally-invasive medical techniques aim to reduce the amount extraneous tissues that are damaged during diagnostic and surgical procedures. This will result in a reduction of patient recovery times, discomfort, as well as deleterious side effects. Minimally invasive surgery can reduce post-operative hospitalization times. The average hospital stay after a standard procedure is usually much longer than for a minimally-invasive procedure. Using minimally-invasive techniques more often could result in millions of dollars saved each year. Although many of the US surgeries could be performed minimally, they are not being done. This is due to the limitations of minimally-invasive instruments and the extra training required for mastering these techniques.
Minimally-invasive robotic surgery or telesurgical system have been developed to improve a surgeon’s hand dexterity, and avoid some limitations of traditional minimally invasive methods. In telesurgery the surgeon manipulates surgical instruments using a remote control, such as servomechanism, instead of holding the instruments and moving them by hand. The surgeon can view an image of the surgery site on a workstation in telesurgery. The surgeon can perform surgical procedures by manipulating master controls while viewing a two-dimensional or three-dimensional image on a display.
The surgical instrument can be supported in a variety of ways during robotic surgery. The slave or driven linkage is also known as the slave. The robotic surgical manipulator is also known as a robot. In U.S. Pat. Nos. Nos. These linkages are often arranged in a parallelogram to hold an object with a shaft. A manipulator can restrict movement so that an instrument pivots around a remote center for manipulation located in space along the length the rigid shaft. The manipulator linkage can be used to position the end effector of a surgical instrument safely. This is done by aligning the remote centre of manipulation with an incision point at the internal surgical site, such as a trocar on an abdominal wall when performing laparoscopic surgery. U.S. Pat. describes alternative manipulator structures. Nos. Nos.
A number of structural arrangements may also be used to position and support the robotic surgical manipulator at the surgical site when performing robotic surgery. Supporting linkage mechanism, also known as set-up joints or set-up arm, is often used to align and position each manipulator to the incision point on a patient. The supporting linkage mechanisms facilitate the alignment of a surgeon’s manipulator to a desired surgical point and targeted anatomy. U.S. Pat. describes exemplary supporting linkage mechanism. Nos. Nos.
While the new telesurgical devices and systems have proved highly effective and beneficial, further improvements are desired.” It is desirable to have improved robotic minimally invasive surgery systems. In some cases, the use of a Telesurgical Device is stopped mid-procedure and requires rehoming after restart. This would be especially beneficial if these systems could safely and efficiently execute a mid procedure restart.
Many embodiments are related to a telesurgery device comprising a surgery assembly including a motor and surgical instrument. The motor can drive at least one of the surgical assembly’s drive mechanisms. A sensor assembly may be connected to non-volatile memories. The sensor assembly is used to record the position of at least one rotating mechanism into the non-volatile storage. The sensor assembly can be connected to a controller. At least one processor can be included in the controller. In many embodiments, the method is also executable by at least one processor. The method records the rotational position during the use of the surgical apparatus of at least one drive mechanisms in the non-volatile storage. The surgical assembly will then be shut down mid-procedure to prevent its use. The request to restart the surgical assembly mid-procedure is received. The mid-procedure start is allowed to proceed if the post-shutdown of at least one of the drive mechanisms is within the accepted tolerance compared to the pre-shutdown of the drive mechanism. The use of the surgical assembly can be allowed or prohibited based on whether the post shutdown position of at least one driving mechanism is within an acceptable tolerance with respect the pre shutdown position of at least one driving mechanism.
In many embodiments, validating the authenticity of the rotational post-shutdown position is part of determining if the position of at least one drive mechanisms is within the acceptable tolerance.
In many embodiments, checking the identity of the surgical tool is part of validating the rotational position before shutting down.
In many embodiments the tolerance accepted is +/- 90 degrees.
The sensor assembly can include a sensor that records a motor assembly’s first rotational location at a position before the gearbox. A second sensor is used to record the second rotational location of the motor at a position after the gearbox. Comparing the ratio of rotations from the first rotational to the second rotational positions is one way of determining whether the rotational post-shutdown position of at least one drive mechanisms is within acceptable tolerance.

In many embodiments, at least one rotatable device is coupled with a rotatable shaft of an instrument.
In many embodiments it is determined that after shutdown, the rotational position at least of one drive mechanism does not fall within the acceptable tolerance. As a result, the controller prevents the further use of surgical assembly.
In many embodiments, a controller will prevent further use of a surgical assembly until a surgical instrument has been demounted from the assembly and mounted again or until remounting the instrument to the assembly is completed.
The detailed description and drawings accompanying the detailed description will help you better understand the nature and benefits of the invention. The drawings and detailed descriptions that follow will reveal other aspects, objects and benefits of the invention.
In the following description will be various embodiments of this invention. To provide a better understanding of embodiments, certain configurations and specific details are provided for the purpose of explanation. It will be obvious to those skilled in the art, however, that the present invention can be implemented without the specifics. In addition, well-known elements may be omitted to avoid obscuring the embodiment described.
Minimally Invasive Robotic Surgery
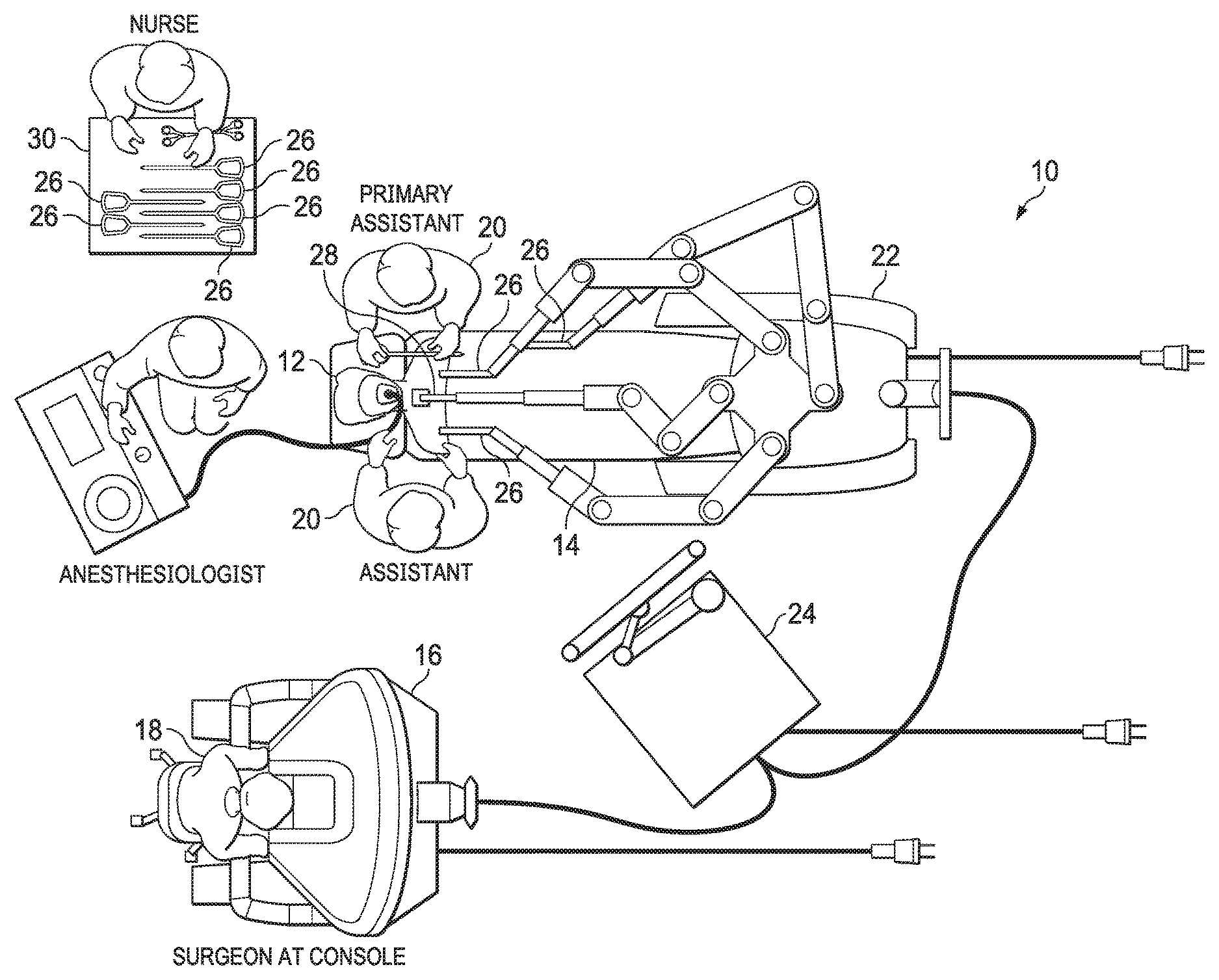
Referring to the drawings in which the same reference numbers represent the same parts throughout all the views. FIG. FIG. 1 shows a plan illustration of a Minimally Invasive Robotic Surgical System (MIRS), which is typically used to perform a minimally invasive surgical or diagnostic procedure on a patient 12 lying on an operating table 14. A Surgeon’s console 16 can be included in the system for use by an Surgeon 18. A Surgeon 18 may be assisted by one or more Assistants. The MIRS system can also include a Patient side cart 22 (surgical robotic) and an Electronics Cart 24. The Patient Side Cart can control at least one removably-coupled tool assembly 26. Through a minimally-invasive incision on the body of the patient 12, the Surgeon 18 can view the surgical site via the Console 16. The Patient Side Cart 22, which is able to manipulate the endoscope 28, can obtain an image of the surgical area. The Electronics Cart 24 is used to process images of the surgical area for display to the Surgeon 18, via the Surgeon Console 16. The number of tools 26 that are used in the operating room at any given time is dependent on a variety of factors, including the type and complexity or the procedure being performed. “If it becomes necessary to replace one or more tools 26 during a procedure an Assistant 20 can remove it from the Patient Side Cart 22 and replace it with a tool 26 on a tray 30 within the operating room.
FIG. The Surgeon’s Console 16 is shown in perspective on FIG. The Surgeon Console 16 has a left-eye display 32 and a display for the right eye 34 that provide the Surgeon with a coordinated stereo image of the surgical site, allowing depth perception. The Console 16 also includes one or multiple input control devices 36 that, in turn, cause the Patient Side Cart 22 to be operated (as shown in FIG. The Console 16 can also include one or more input control devices 36, which in turn cause the Patient Side Cart 22 (shown in FIG. The input control devices can have the same degree of freedom as their corresponding tools 26 (shown on FIG. The Surgeon can be provided with telepresence or the feeling that the input controls 36 are integrated with the tools 26, so that he feels like he is directly controlling them. In order to achieve this, position, tactile feedback, and force sensors (not shown) can be used to transmit the position, tactile sensations, and force from the tools 26 to the Surgeons hands via the input control devices.
The Surgeon’s Console 16, which is located in the same area as the Patient, allows the Surgeon to monitor the procedure directly, be physically present, if needed, and communicate directly with an Assistant rather than using a telephone or another communication medium. The Surgeon may be in a different location, such as a different building or room from the patient, to allow for remote surgery.
FIG. The Electronics Cart 24 is shown in perspective on FIG. The Electronics Cart 24 is coupled to the endoscope 28, and includes a processor that processes captured images to be displayed to the surgeon on the console or another display locally or remotely. The Electronics Cart 24 may, for example, process captured images when a stereoscopic scope is used to provide coordinated stereo images. This coordination can include aligning the images in opposition and adjusting the stereo distance of the endoscope. “Another example of image processing is the use of previously calibrated camera parameters to compensate the imaging errors of the device that captures the images, such as optical distortions.

Click here to view the patent on Google Patents.