Invented by Miriam A. Kelly, Alan M. Lotvin, Medco Health Solutions Inc, Express Scripts Strategic Development Inc
The method for care assessment and management involves a systematic approach to evaluating the needs of patients and developing a care plan that addresses those needs. This approach takes into account the patient’s medical history, current health status, and any other factors that may impact their care. It also involves ongoing monitoring and adjustment of the care plan as needed.
One of the key benefits of this method is that it helps healthcare providers identify patients who are at risk for complications or readmission to the hospital. By identifying these patients early on, providers can intervene to prevent complications and reduce the need for costly hospital readmissions.
Another benefit of the method for care assessment and management is that it helps providers coordinate care across different settings and providers. This is particularly important for patients with complex medical needs who may receive care from multiple providers in different locations. By coordinating care, providers can ensure that patients receive the right care at the right time, reducing the risk of medical errors and improving outcomes.
The market for this method is expected to continue to grow as healthcare providers seek to improve the quality of care while reducing costs. In addition, the shift towards value-based care models, which reward providers for improving outcomes and reducing costs, is driving demand for this approach.
There are a number of companies that offer solutions for care assessment and management, including software platforms and consulting services. These companies are working to develop innovative solutions that can help providers improve care while reducing costs.
Overall, the market for method for care assessment and management is poised for significant growth in the coming years. As healthcare providers continue to seek ways to improve outcomes and reduce costs, this approach will become increasingly important in delivering high-quality, cost-effective care.

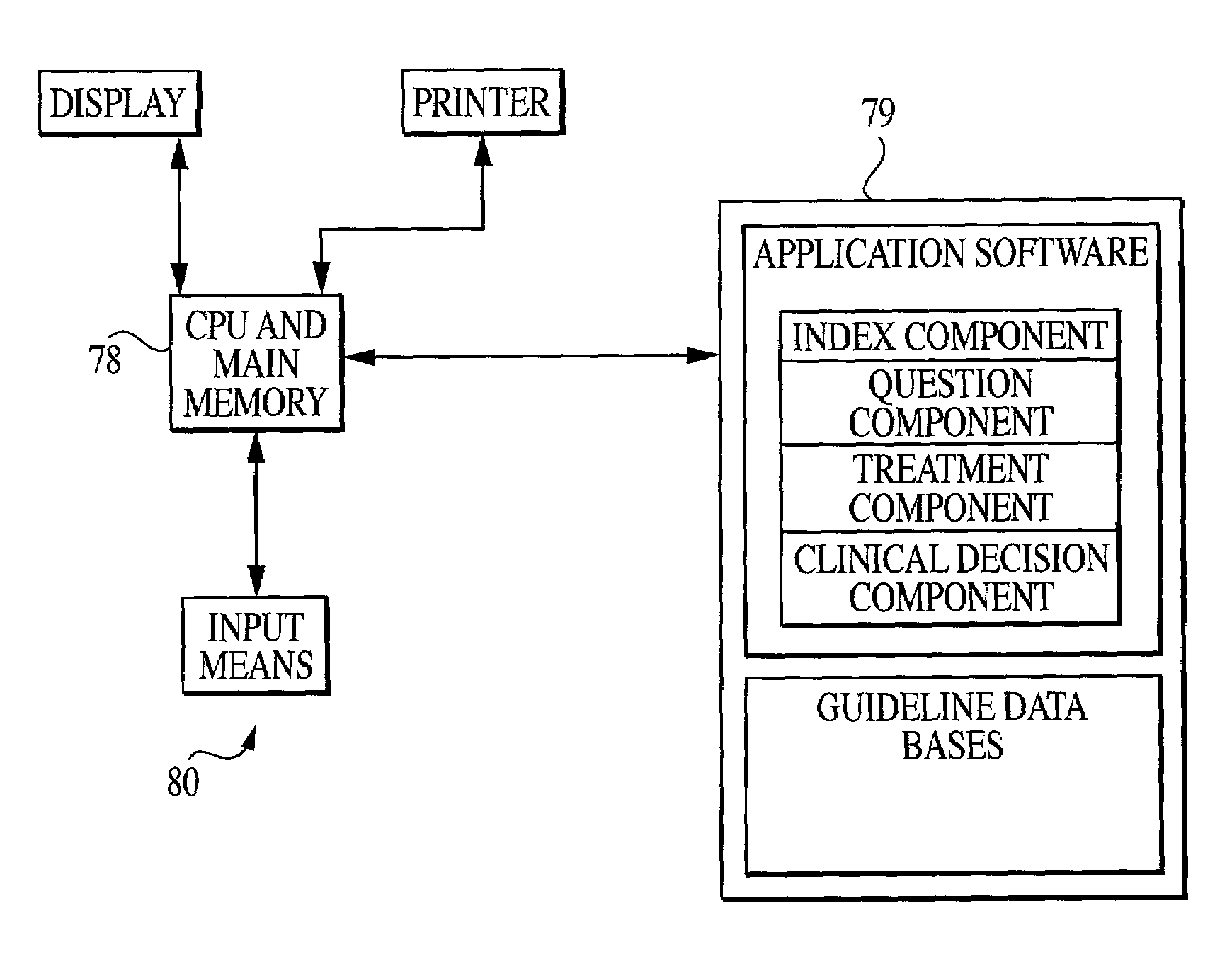
The Medco Health Solutions Inc, Express Scripts Strategic Development Inc invention works as follows
An interactive computer-assisted method” compiles comprehensive patient health information in a central repository. It then assesses and analyses this information and identifies the high users of health services by using a computer with a user. The method comprises the steps of creating an integrated repository containing various databases of patient information including demographics and behavior and optionally, the results of core surveys of health status questions. Optionally, the invention includes the steps of determining core questions as well as criteria for deciding whether or not to ask specific questions to particular patients depending on their responses to previous questions. The invention predicts accurately the risk of a condition or its progression using an interactive administration of core survey question combined with diagnostic data. Patients are placed efficiently, reliably and accurately in the appropriate treatment interventions programs. The invention eliminates repetitive, redundant surveying of multiple medical conditions patients.

Background for Method for care assessment and management
1. “1.
The present invention is a computer-implemented and/or assisted method for one or more of the following: eliminating redundant, repetitious surveying of multiple medical conditions in patients, identifying high resource users in a population for health care, improving clinical data for use in drug utilization review, prior authorization and care management programs, or identifying likely candidates to participate in other health management programs. This can be done while maintaining or improving quality of care for a patient population. The present invention is more specifically a computer-implemented and/or assisted method for creating a comprehensive profile of a patient using, among other information sources, medical claims, drug claim files, and interactive selection and/or gathering of extensive information about a patient’s health status, demographics and risk behavior. The present invention relates also to assisting in real time, if desired, with the identification of possible drug-disease or drug-drug side effects. The present invention facilitates delivery of high-quality care by combining diagnosis information, vital statistics information and drug claims related information from various internal and external databases and sources.
2. “2.
Health care costs are still a large part of the Gross National Product in the United States and they continue to rise. Drug utilization reviews (DUR) are one of the programs that help contain health care costs. Prior authorization of medical treatment, programs that allow patients to receive diagnostic advice about specific problems directly from the doctors and programs that identify and use intervention programs to prevent future problems or disease progression are all part of the health care cost containment programs.
A significant part of these costs are attributed to people who use health care services more than the average. The lack of knowledge about the likely needs and nature of high-risk health care users makes it difficult to tailor interventions and address their medical needs.
The administrative costs of enrolling patients with high levels of inappropriate use in intervention programs have been high. This is partly because patients who are enrolled in these programs must complete multiple questionnaires to assess their overall health. These surveys or questionnaires are costly and burdensome for the program. Some of the questionnaires are designed to assess health risks, but they do not predict future resource usage.
We have found that many patients do not receive the best health care information and programs, because they are not available in a practical way. Many people are delaying or avoiding seeking medical attention due to cost, time restrictions, or inconvenience. Many diseases could be treated more efficiently and effectively if health management programs were able to access updated information about the medical condition and health management needs of patients. Early detection and treatment could also prevent or delay the progression of many diseases. The costs of treating these advanced stages of disease are significant.
The inventors state that there is no prior art to date which they are aware of, that integrates survey data and diagnostic data into an integrated model for high resource utilization. They also note the lack of a central database of patient data, for assessing the impact of health management programs. These other programs will be described in order to provide background information.
There are several problems with this type of system. These systems are expensive because a nurse must answer every telephone call. The caller might have to be a member of a health plan that offers the service to use it. This system, which is designed for reactive problems, does not allow the caller to prevent or eliminate such conditions from happening in the first place. These advice systems cannot be implemented for large populations of patients, especially when the proactive measures are specific to each patient.
There are other inventions available such as an automated service that provides health care advice and answers questions in the home. This service may be provided by a health maintenance organization to its members within a specific geographic area. HMO members can get advice from home by connecting a small box to their telephone and calling a toll free number. The user enters answers to questions on the screen using a keyboard built into the box. According to the answers given, the user may be instructed to use a home remedy or to call a doctor or nurse. They might also be given an appointment for an examination. This system, like Ask-A-Nurse, is designed to react to problems that are determined by the caller. It does not provide the ability to prevent such conditions from occurring.

At the opposite end, there are various attempts to analyze retroactively, using hindsight the appropriateness and cost of the medical care delivered. U.S. Pat. No. No. Leatherman et al .).
The process is usually performed on the request of customers who are a health maintenance organisation, indemnity insurance (e.g. Blue Cross), large self-insured employers groups or government programs (e.g. Medicaid). The process starts by gathering the parameters specific to the client, such as the time period they wish to analyze or if they want to break down data by providers or any other grouping variables. Next, the system parameters and options are updated based on the customer’s specifications. The system then loads and obtains the customer data 3. This data is usually comprised of a customer’s computerized health care claims for a specific period, along with enrollment and health care provider information.
The enrollment data is extracted 4 to identify enrollees that are served by the client and meet a predefined criteria for enrollment. The enrollment data consists of one record for each enrollee. Then, relevant claims data is extracted from the entire customer data base 5, and configured via linkages to create the necessary health records. “The claims data include claims for medical professional service (outpatient records), claims for hospital services, (inpatients records), and pharmacy records (pharmacy record).
If the customer so desires, provider-specific information is also extracted. This allows the analysis to be further broken down according to the specific provider of products or services, such as a doctor, clinic, or hospital. The files that result are then merged into uncorrected masters files. Claims that are duplicates and those that have been reversed by the claims adjudication are excluded. This creates a master record of health care claim records.
This prior art involves also the application of definitions for health care conditions to identify the population with that condition. Then, an analysis of claims records for this population (a subset from the master files) is performed under the quality care criteria defined 12 (FIG. 2).
The report will include: a written report from the perspective of quality care, a statistical analysis that is worthy of attention, and recommendations to improve the quality of health care.
The software 16 and the described process produce charts, graphs and reports. Using the next definition of a health care condition to identify the population with that condition and then an analysis is performed on the claims records from that population using the quality care criteria defined for the next condition. The reports are then compiled into a quality report for each condition. This is presented to customers 17 after all specified health conditions have been processed.
The system determines if detailed analysis is required.” No further data is collected or analyzed if there is no need for detailed analysis. If a detailed analysis is needed for a health condition, a sample of the population with that condition will be used to identify which enrollees need to have additional medical records collected. 3). The medical records of the patient are abstracted, with the consent of the provider, focusing on the events that pertain to the specific health condition being studied. This results in a medical records abstract form 19.
This abstracted data is then input into the system using a computer to create a medical records abstract data file. The charts and graphs report the statistically observed data for the population that is defined as having the condition of health interest. A report with recommendations to improve the quality of health care services can also be generated. 4). If a detailed analysis of records for multiple conditions is required, the steps above are repeated until charts or graphs displaying statistically observed data are created and a report with recommendations to improve quality in health care for each condition 22.
The process is complete once all of the health conditions are processed. This system has a major flaw, which is that it analyses ‘after the fact’. The appropriateness of medical care delivered in terms of quality and cost. Leatherman et al. The system focuses on the appropriateness and cost of the medical service and does not consider patient specific treatment or future/proactive treatments prior to the occurrence of medical conditions.

Click here to view the patent on Google Patents.