Invented by Kevin J. Tracey, Jared M. Huston, North Shore Long Island Jewish Research Institute, Feinstein Institute for Medical Research
Inflammatory cytokines play a crucial role in the body’s immune response, helping to regulate the inflammatory process and fight off infections. However, when the immune system becomes dysregulated, excessive production of these cytokines can lead to chronic inflammation, which is associated with a wide range of diseases, including autoimmune disorders, cardiovascular diseases, and neurodegenerative conditions.
Cholinergic antagonists, also known as anticholinergic drugs, are a class of medications that block the action of acetylcholine, a neurotransmitter involved in various physiological processes, including inflammation. By inhibiting the cholinergic system, these drugs can help reduce the production of inflammatory cytokines and dampen the immune response.
Vagus nerve stimulation (VNS) is another approach that has gained attention in recent years. The vagus nerve is a major component of the parasympathetic nervous system, which helps regulate various bodily functions, including inflammation. By stimulating the vagus nerve, either through electrical impulses or pharmacological means, researchers have found that they can modulate the immune response and reduce inflammation.
The market for inhibition of inflammatory cytokines by cholinergic antagonists and vagus nervous stimulation is driven by the increasing prevalence of chronic inflammatory diseases and the need for more effective treatment options. Pharmaceutical companies are investing heavily in research and development to identify novel cholinergic antagonists and develop innovative vagus nerve stimulation techniques.
Several clinical trials have already demonstrated the potential of these approaches in various disease conditions. For example, in rheumatoid arthritis, a chronic autoimmune disorder characterized by joint inflammation, cholinergic antagonists have shown promising results in reducing disease activity and improving symptoms.
In addition to rheumatoid arthritis, cholinergic antagonists and vagus nerve stimulation are being explored as potential treatments for other inflammatory conditions, such as inflammatory bowel disease, asthma, and neuroinflammatory disorders like multiple sclerosis and Alzheimer’s disease.
However, despite the promising results, there are still challenges to overcome in this market. One of the main challenges is the development of targeted therapies that selectively inhibit inflammatory cytokines without affecting other physiological processes regulated by the cholinergic system. This specificity is crucial to minimize potential side effects and ensure the safety and efficacy of these treatments.
Another challenge is the optimization of vagus nerve stimulation techniques. While VNS has shown promising results in preclinical and early clinical studies, further research is needed to determine the optimal parameters for stimulation and identify patient populations that would benefit the most from this approach.
In conclusion, the market for inhibition of inflammatory cytokines by cholinergic antagonists and vagus nervous stimulation is a rapidly evolving field with significant potential for the development of novel therapies. As research continues to uncover the underlying mechanisms of inflammation and immune regulation, pharmaceutical companies are poised to capitalize on this market and provide patients with more effective and targeted treatments for chronic inflammatory diseases.
The North Shore Long Island Jewish Research Institute, Feinstein Institute for Medical Research invention works as follows
A method for inhibiting the release a proinflammatory cell cytokine is disclosed. The cell is treated with a cholinergic receptor agonist. This method can be used in patients who are at risk of, or suffer from, an inflammatory cascade mediated by cytokines, such as endotoxic shock. The cholinergic-agonist treatment is effected either by stimulating an efferent nerve fiber or the entire vagus nervous system.
Background for Inhibition inflammatory cytokine by cholinergic antagonists and vagus nervous stimulation
1. “1.
The present invention is a method of reducing inflammation. The invention is more specifically a method for reducing inflammation that is caused by proinflammatory molecules or an inflammatory cascade.
2. “2.
Vertebrates maintain internal homeostasis in the face of infection or injury, by balancing proinflammatory and antiinflammatory pathways. In many diseases, however, this internal balance is disturbed. “For example, the endotoxin, lipopolysaccharide (LPS), produced by Gram-negative bacteria, activates macrophages and releases cytokines which are potentially fatal (44; 10); 47; 31).
Or cachectin), interleukin (IL)-1.alpha., IL-1.beta., IL-6. IL-8. L-18. Interleukin-1.alpha. IL-1.beta. IL-6, IL-8, L-18, cachectin, interleukin-1.beta. IL-1.alpha. IL-1.beta. IL-1.beta. IL-1.alpha. IL-1.beta. IL-6, IL-8, L-18, interferony, platelet activating factor (PAF), mac Other compounds such as high mobility group 1 (HMG-1) are also induced in conditions like sepsis, and can serve as proinflammatory molecules (57). These proinflammatory cells are produced by a variety of cell types. The most important being immune cells like monocytes, neutrophils, macrophages, but also non-immune ones such as fibroblasts (for instance, smooth muscle cells), osteoblasts (for example, osteoblasts), epithelial (for example, neurons), and fibroblasts (for instance, monoocytes). “Proinflammatory cytokines are responsible for various diseases, including sepsis. They release inflammatory cytokines during a cascade of cytokines.
In Included are disorders characterized by both localized and systemic reactions, including, without limitation, diseases involving the gastrointestinal tract and associated tissues (such as appendicitis, peptic, gastric and duodenal ulcers, peritonitis, pancreatitis, ulcerative, pseudomembranous, acute and ischemic colitis, diverticulitis, epiglottitis, achalasia, cholangitis, coeliac disease, cholecystitis, hepatitis, Crohn’s disease, enteritis, and Whipple’s disease); systemic or local inflammatory diseases and conditions (such as asthma, allergy, anaphylactic shock, immune complex disease, organ ischemia, reperfusion injury, organ necrosis, hay fever, sepsis, septicemia, endotoxic shock, cachexia, hyperpyrexia, eosinophilic granuloma, granulomatosis, and sarcoidosis); diseases involving the urogential system and associated tissues (such as septic abortion, epididymitis, vaginitis, prostatitis and urethritis); diseases involving the respiratory system and associated tissues (such as bronchitis, emphysema, rhinitis, cystic fibrosis, adult respiratory distress syndrome, pneumonitis, pneumoultramicroscopicsilicov- -olcanoconiosis, alvealitis, bronchiolitis, pharyngitis, pleurisy, and sinusitis); diseases arising from infection by various viruses (such as influenza, respiratory syncytial virus, HIV, hepatitis B virus, hepatitis C virus and herpes), bacteria (such as disseminated bacteremia, Dengue fever), fungi (such as candidiasis) and protozoal and multicellular parasites (such as malaria, filariasis, amebiasis, and hydatid cysts); dermatological diseases and conditions of the skin (such as burns, dermatitis, dermatomyositis, sunburn, urticaria warts, and wheals); diseases involving the cardiovascular system and associated tissues (such as vasulitis, angiitis, endocarditis, arteritis, atherosclerosis, thrombophlebitis, pericarditis, myocarditis, myocardial ischemia, congestive heart failure, periarteritis nodosa, and rheumatic fever); diseases involving the central or peripheral nervous system and associated tissues (such as Alzheimer’s disease, meningitis, encephalitis, multiple sclerosis, cerebral infarction, cerebral embolism, Guillame-Barre syndrome, neuritis, neuralgia, spinal cord injury, paralysis, and uveitis); diseases of the bones, joints, muscles and connective tissues (such as the various arthritides and arthralgias, osteomyelitis, fasciitis, Paget’s disease, gout, periodontal disease, rheumatoid arthritis, and synovitis); other autoimmune and inflammatory disorders (such as myasthenia gravis, thryoiditis, systemic lupus erythematosus, Goodpasture’s syndrome, Behcets’s syndrome, allograft rejection, graft-versus-host disease, Type I diabetes, ankylosing spondylitis, Berger’s disease, Type I diabetes, ankylosing spondylitis, Berger’s disease, and Retier’s syndrome); as well as various cancers, tumors and proliferative disorders (such as Hodgkins disease); and, in any case the inflammatory or immune host response to any primary disease (13; 55; 30; 20; 33; 25; 18; 27; 48; 24; 7; 9; 4; 3; 12; 8; 19; 15; 23; 49; 34).
Mammals respond in part to inflammation caused by inflammatory cascades of cytokine mediated cytokine cascades through central nervous system control. This response was characterized with regard to the systemic humoral responses during inflammatory reactions to endotoxins (2, 54, 21; 28). In one response, endotoxin and cytokines activate afferent fibers of the vagus nerve, which stimulates humoral anti-inflammatory responses via glucocorticoid release (51, 41, 39). In previous work, vagus signaling was identified as a key component of the afferent circuit that modulates the fever and adrenocorticotropin responses to systemic cytokinemia and endotoxemia (14, 11; 52;35). “However, relatively little is known about efferent neuronal pathways that modulate inflammation.
Effective vagus nerve signals have been implicated in facilitating the release of lymphocytes from thymus through a nicotinic receptor response. Clinical studies also indicate that nicotine can be an effective treatment for some cases of inflammatory colitis (17; 36) and that the levels of proinflammatory cytokines are reduced in smokers who have inflammatory colitis (40). These findings do not suggest that cholinergic receptor agonists are able to inhibit an inflammatory cascade of cytokines, especially those mediated through macrophages. There is also no evidence in the literature to suggest that stimulation of the efferent Vagus nerve is effective at inhibiting these cascades.
The inventor succeeded in discovering cholinergic antagonists that can inhibit the release proinflammatory cytokines in mammalian cells, either in vitro, or in vivo. This inhibiting effect can be used to stop inflammatory cytokine pathways that are responsible for many diseases. By stimulating the efferent Vagus nerves, cholinergic-agonist treatment can inhibit local or systemic inflammatory cascades.
The In The The In other preferred embodiments, the cell is in a patient suffering from, or at risk for, a condition mediated by an inflammatory cytokine cascade, preferably appendicitis, peptic, gastric or duodenal ulcers, peritonitis, pancreatitis, ulcerative, pseudomembranous, acute or ischemic colitis, diverticulitis, epiglottitis, achalasia, cholangitis, cholecystitis, hepatitis, Crohn’s disease, enteritis, Whipple’s disease, asthma, allergy, anaphylactic shock, immune complex disease, organ ischemia, reperfusion injury, organ necrosis, hay fever, sepsis, septicemia, endotoxic shock, cachexia, hyperpyrexia, eosinophilic granuloma, granulomatosis, sarcoidosis, septic abortion, epididymitis, vaginitis, prostatitis, urethritis, bronchitis, emphysema, rhinitis, cystic fibrosis, pneumonitis, pneumoultramicroscopicsilicovolcanoconiosis, alvealitis, bronchiolitis, pharyngitis, pleurisy, sinusitis, influenza, respiratory syncytial virus infection, herpes infection, HIV infection, hepatitis B virus infection, hepatitis C virus infection, disseminated bacteremia, Dengue fever, candidiasis, malaria, filariasis, amebiasis, hydatid cysts, burns, dermatitis, dermatomyositis, sunburn, urticaria, warts, wheals, vasulitis, angiitis, endocarditis, arteritis, atherosclerosis, thrombophlebitis, pericarditis, myocarditis, myocardial ischemia, periarteritis nodosa, rheumatic fever, coeliac disease, congestive heart failure, adult respiratory distress syndrome, Alzheimer’s disease, meningitis, encephalitis, multiple sclerosis, cerebral infarction, cerebral embolism, Guillame-Barre syndrome, neuritis, neuralgia, spinal cord injury, paralysis, uveitis, arthritides, arthralgias, osteomyelitis, fasciitis, Paget’s disease, gout, periodontal disease, rheumatoid arthritis, synovitis, myasthenia gravis, thryoiditis, systemic lupus erythematosus, Goodpasture’s syndrome, Behcets’s syndrome, allograft rejection, graft-versus-host disease, Type I diabetes, ankylosing spondylitis, Berger’s disease, Type I diabetes, ankylosing spondylitis, Berger’s disease, Retier’s syndrome, or Hodgkins disease. The The In The It You Direct
The The The cholinergic agonist is preferably acetylcholine, nicotine, muscarine, carbachol, galantamine, arecoline, cevimeline, or levamisole, and the condition is preferably appendicitis, peptic, gastric or duodenal ulcers, peritonitis, pancreatitis, ulcerative, pseudomembranous, acute or ischemic colitis, diverticulitis, epiglottitis, achalasia, cholangitis, cholecystitis, hepatitis, Crohn’s disease, enteritis, Whipple’s disease, asthma, allergy, anaphylactic shock, immune complex disease, organ ischemia, reperfusion injury, organ necrosis, hay fever, sepsis, septicemia, endotoxic shock, cachexia, hyperpyrexia, eosinophilic granuloma, granulomatosis, sarcoidosis, septic abortion, epididymitis, vaginitis, prostatitis, urethritis, bronchitis, emphysema, rhinitis, cystic fibrosis, pneumonitis, pneumoultramicroscopicsilicovolcanoconiosis- -, alvealitis, bronchiolitis, pharyngitis, pleurisy, sinusitis, influenza, respiratory syncytial virus infection, herpes infection, HIV infection, hepatitis B virus infection, hepatitis C virus infection, disseminated bacteremia, Dengue fever, candidiasis, malaria, filariasis, amebiasis, hydatid cysts, burns, dermatitis, dermatomyositis, sunburn, urticaria, warts, wheals, vasulitis, angiitis, endocarditis, arteritis, atherosclerosis, thrombophlebitis, pericarditis, myocarditis, myocardial ischemia, periarteritis nodosa, rheumatic fever, Alzheimer’s disease, coeliac disease, congestive heart failure, adult respiratory distress syndrome, meningitis, encephalitis, multiple sclerosis, cerebral infarction, cerebral embolism, Guillame-Barre syndrome, neuritis, neuralgia, spinal cord injury, paralysis, uveitis, arthritides, arthralgias, osteomyelitis, fasciitis, Paget’s disease, gout, periodontal disease, rheumatoid arthritis, synovitis, myasthenia gravis, thryoiditis, systemic lupus erythematosus, Goodpasture’s syndrome, Behcets’s syndrome, allograft rejection, graft-versus-host disease, Type I diabetes, ankylosing spondylitis, Berger’s disease, Type I diabetes, ankylosing spondylitis, Berger’s disease, Retier’s syndrome, or Hodgkins disease. The The The
In additional embodiments, this invention is directed at a method of treating a patient who suffers from or is at risk of a condition caused by an inflammatory cascade. The method includes stimulating the vagus nerve efferent activity in the patient to the extent necessary to inhibit the cascade of inflammatory cytokines. The preferred methods of stimulation, and the preferred conditions are similar to those described previously.
In other embodiments of the invention, a method is provided for attenuating a systemic inflammation response in a patient to an endotoxin. The method includes stimulating the efferent nerve activity of a patient to an extent that inhibits an inflammatory cascade.
The present invention also relates to a method of determining if a compound is an cholinergic receptor agonist. The method includes determining if the compound inhibits a release of proinflammatory cytokine by a mammalian cellular. In preferred embodiments, the cell is a mammalian macrophage. The proinflammatory cytokine in this case is TNF.
The practice will use, unless otherwise specified, conventional techniques in cell culture, molecular biochemistry, microbiology and cell biology. These are within the scope of the current art.” These techniques are explained in detail in the literature. See, e.g., Sambrook et al., 1989, ?Molecular Cloning: A Laboratory Manual?, Cold Spring Harbor Laboratory Press; Ausubel et al. “Short Protocols in Molecular Biology”, John Wiley and Sons, 1995; Methods in Enzymology and Cell Biology (several Volumes); and Methods in Molecular Biology.
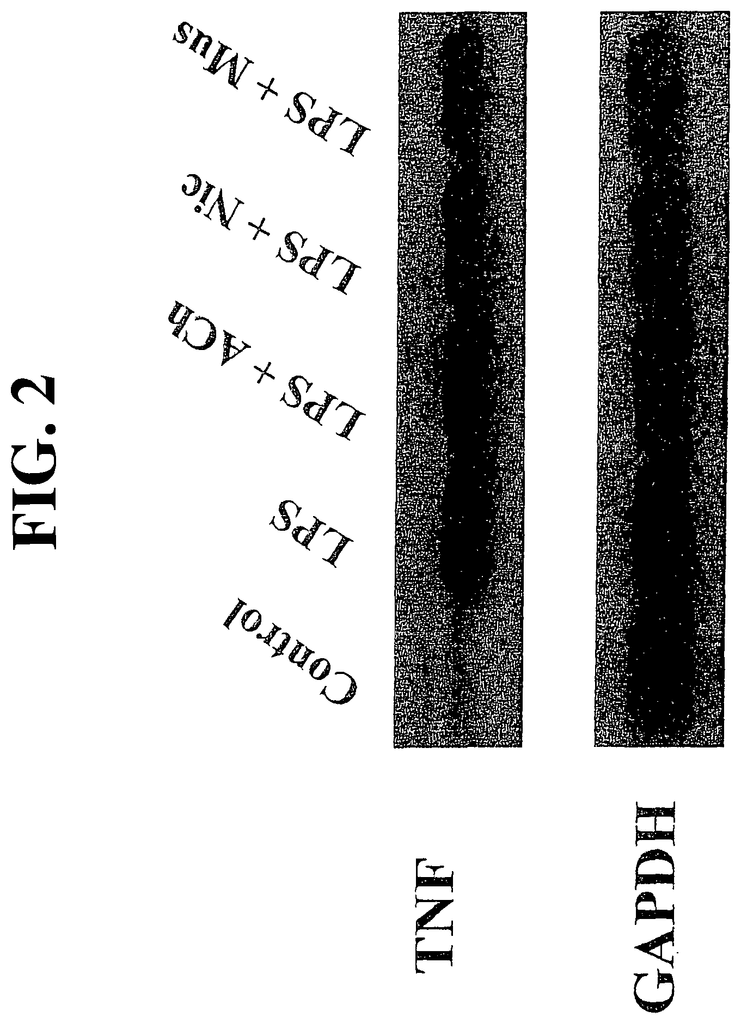
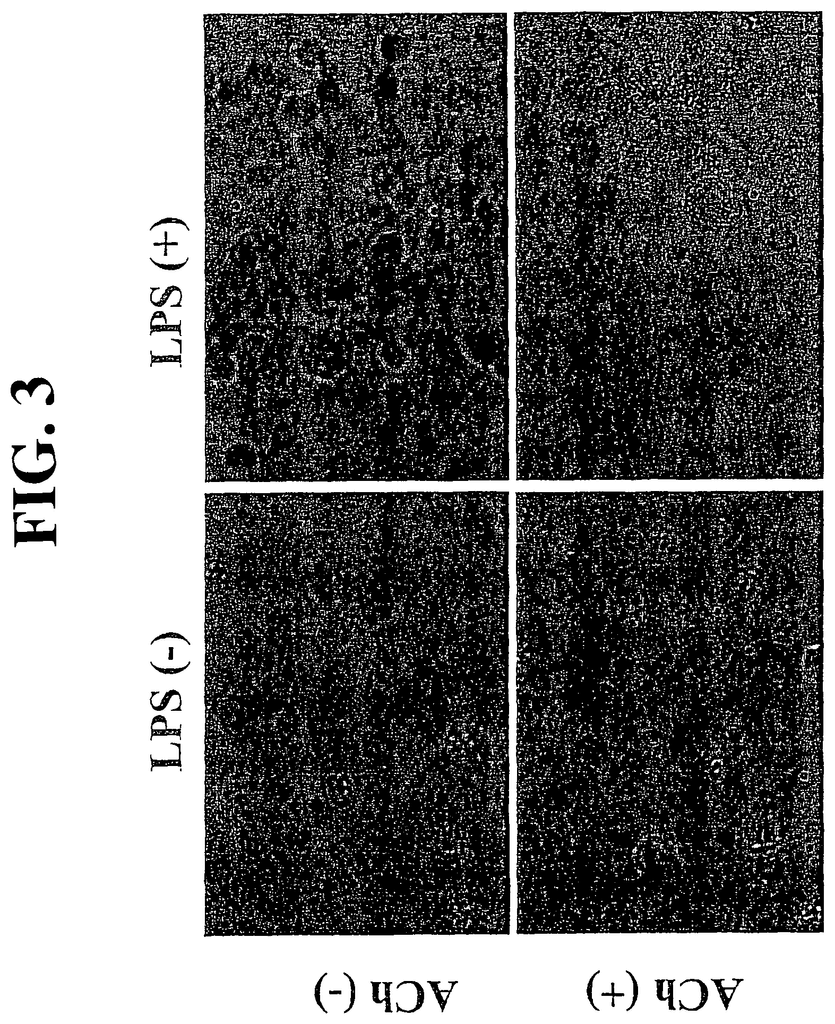
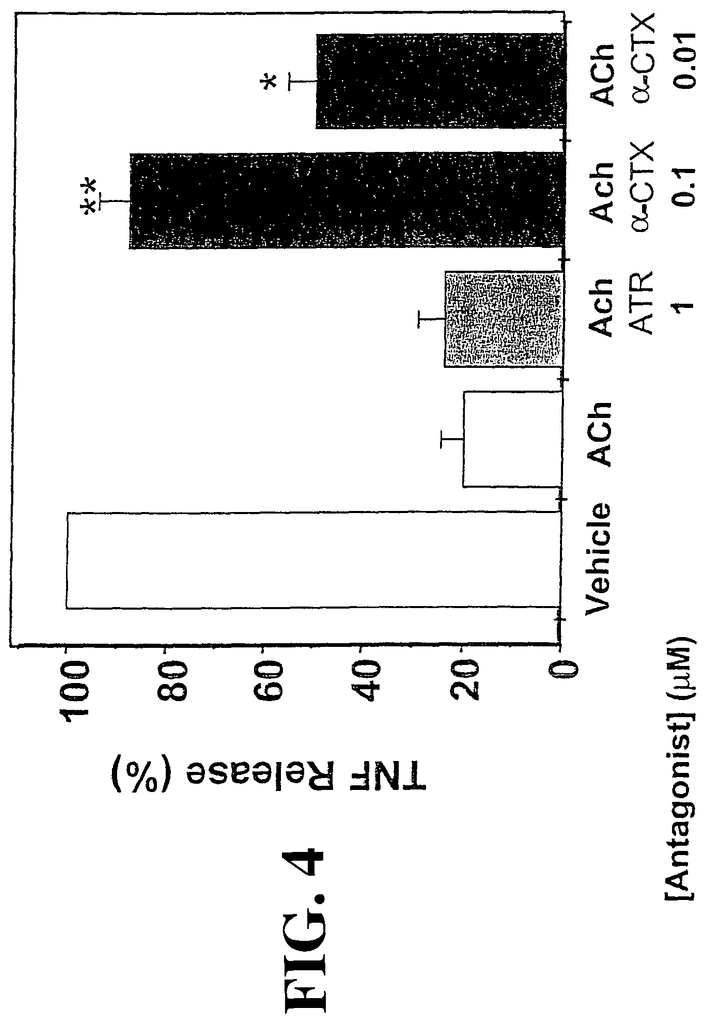
The present invention is based upon the discovery that treatment with a cholinergic-agonist of a cell that produces proinflammatory molecules attenuates their release, and that the attenuation can be used to treat disorders caused by an inflammatory cascade (5-6). The stimulation of the efferent nerve fibers released enough acetylcholine in order to stop an inflammatory cascade systemic, such as that seen in endotoxic shock (5), or localized. The stimulation of the efferent nerve can also inhibit localized inflammatory cascades in tissues and organs served by efferent nerve fibers.
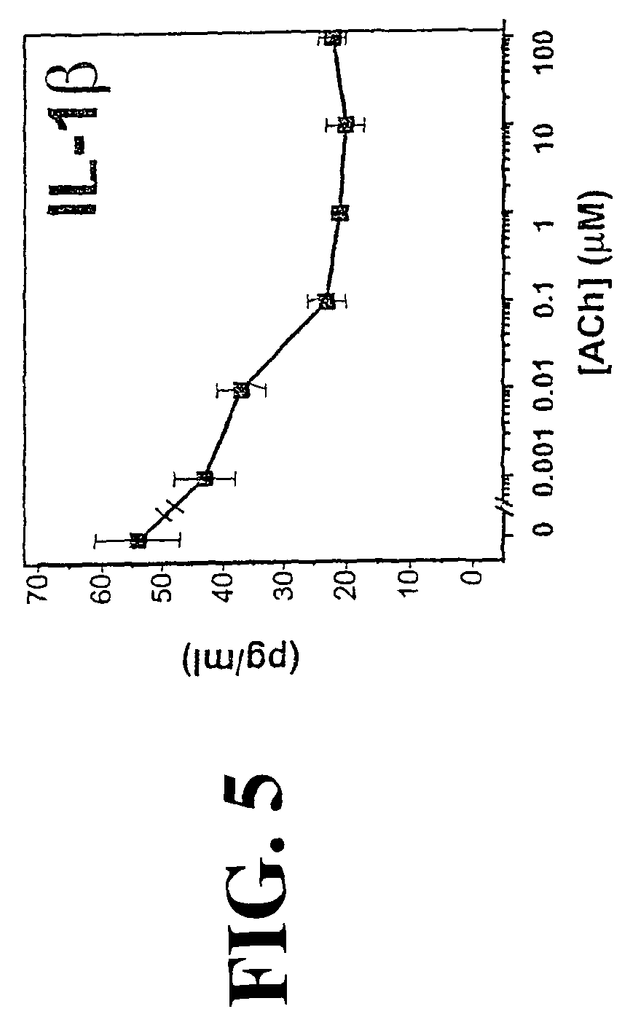
The present invention, according to some embodiments, is directed at methods for inhibiting the release a proinflammatory cell from a mammalian. The methods include treating the cell in a sufficient amount with a cholinergic receptor agonist to reduce the amount of proinflammatory cytokine that is released by the cell.
As used in this document, a “cytokine” is a soluble peptide or protein that is produced naturally by mammalian cell and that acts as a humoral regulator at concentrations between micro- to picomolar. Under normal or pathological circumstances, cytokines can modulate the function of cells and tissues. Proinflammatory cytokines are cytokines that can cause any of the physiological reactions associated to inflammation, including vasodialation and hyperemia. They may also increase permeability in vessels, causing edema or granulocytes. In some cases the proinflammatory cytokine may also trigger apoptosis. For example, TNF can stimulate cardiomyocyte death in chronic heart failure (32;45). Proinflammatory cytokines include, but are not limited to, tumor necrosis (TNF), interleukin-1.alpha. IL-1.beta. IL-6 IL-8 IL-18 interferon.gamma. HMG-1 platelet activating factor (PAF), macrophage migration inhibiting factor (MIF). In preferred embodiments, the proinflammatory cytokine inhibited by cholinergic agonists is TNF, IL-1 or IL-18. This is because these cytokines, produced by macrophages, are responsible for many serious disorders such as endotoxic shock and asthma. The proinflammatory cytokine in most preferred embodiments is TNF.
Proinflammatory cytokines must be distinguished from non-inflammatory cytokines such as IL-4 and IL-10. Cholinergic agonists do not inhibit the release of anti-inflammatory molecules in preferred embodiments.
In many cases, proinflammatory molecules are released in an inflammatory cascade. This is defined as the in-vivo release of one or more proinflammatory cytokines in a mammal. The cytokine releases affect the physiological condition of the animal. In embodiments of the invention, an inflammatory cascade is inhibited when proinflammatory cytokine releases cause a deleterious condition.
Any mammalian cells that produce proinflammatory cytokines is useful for the practice the invention.” Examples include monocytes (macrophages), neutrophils (neutrophils), epithelial and neuronal cells as well as osteoblasts, fibroids, fibroblasts and fibroblasts. In preferred embodiments the cell is macrophage.
Click here to view the patent on Google Patents.