Invented by Nortman; Scott, Jassir; David, Restful Robotics, Inc.
**Blog Title: The Future of Sleep Apnea Therapy: Robotic Arm Systems for Automatic PAP Mask Placement**
**Introduction**
Obstructive Sleep Apnea (OSA) is a pervasive health issue that affects millions globally, leading to a host of downstream health problems, from chronic fatigue and impaired cognitive function to increased risks of hypertension, cardiovascular disease, and stroke. The gold standard for OSA management remains positive airway pressure (PAP) therapy, including CPAP (continuous PAP), APAP (automatic PAP), and BPAP (bilevel PAP) devices. Despite their efficacy, a striking percentage of patients struggle with compliance, largely owing to issues with mask discomfort, improper fit, anxiety, and other psychological barriers associated with nighttime mask use.
Enter the cutting-edge robotic arm system: a recently disclosed invention that leverages robotics, computer vision, and biometric data to automate and optimize the placement and continual adjustment of PAP masks, addressing a core barrier to effective OSA care. In this comprehensive blog post, we’ll analyze the invention’s functionality and its potential to revolutionize not just sleep medicine, but adjacent sectors of healthcare. We’ll also explore market opportunities and estimate the technology’s Total Addressable Market (TAM) and Serviceable Addressable Market (SAM).
—
### **Summary of the Invention: A Smarter, Safer Way to Deliver PAP Therapy**
The system at the heart of this innovation consists of several interlinked components:
– **Robotic Arm & Flange**: A dexterous robot arm, capable of fine, multi-axis movement, is stationed at the patient’s bedside. At its end is a flange designed to couple with various mask types (nasal, oral, full-face).
– **Mask and Ventilator Integration**: The robot arm holds the mask, which is connected via a gas tube to a ventilator delivering positive airway pressure.
– **Controllers and Sensors**: These orchestrate precise robot motion, monitor and adjust mask positioning, and regulate gas flow.
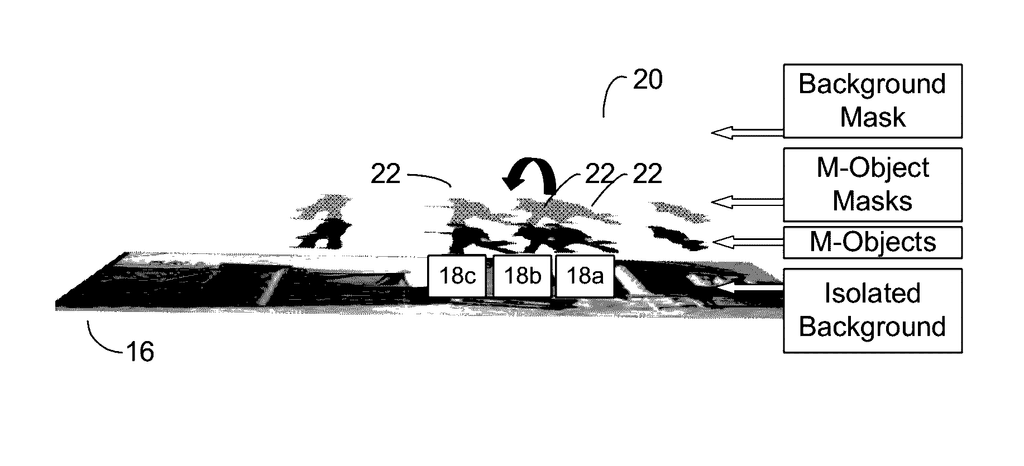
– **Computer Vision System**: Cameras (potentially infrared, NIR, or LiDAR) track the patient’s facial landmarks in real time, ensuring the mask aligns perfectly—even as the patient moves in their sleep.
– **Biometric Monitoring**: Wearable sensors (like wristbands) or robot-integrated sensors gather vital biometrics, such as heart rate, motion, oxygen saturation, and sleep state. The system can time mask placement (e.g., waiting until the user is asleep to apply the mask) and automatically adjust pressure or force for optimal comfort.
– **RFID or ID Systems**: Used for tracking mask and tubing types, for hygiene compliance, and for pairing disposable accessories with appropriate patients or therapy sessions.
The operation is governed by a sophisticated state machine, orchestrating transitions like booting, idling, readiness, waiting for sleep, sleep detection, mask approach, seating, force maintenance, retraction, and error handling.
**What does all this mean in practice?** PAP users can go to bed without strapping on a mask. As the system detects they are asleep, the robotic arm gently positions and seats the mask with just the right pressure, automatically maintaining a secure seal even as they shift in bed. Should the user wake or require intervention, the system retracts the mask, minimizing disruption and anxiety. By handling mask placement and adjustment, this technology promises to surmount key hurdles in PAP therapy adherence.
—
### **Potential Applications: Beyond Sleep Apnea**
While the initial development targets OSA and PAP therapy, the architecture and adaptability of this robotic arm system lend themselves to a broad range of clinical and home health uses. Let’s outline the most immediately promising applications:
#### **1. Sleep Apnea Therapy (PAP/CPAP/BPAP/APAP)**
– **Residential Use**: For home-based OSA management—by far the largest user group for PAP devices.
– **Hospital or Sleep Lab Use**: In settings where precise control and monitoring are required, particularly for vulnerable or high-risk populations.
#### **2. Non-Invasive Ventilation (NIV) in Critical Care and Hospitals**
Hospitals often use masks for non-invasive ventilation (for COPD, acute respiratory failure, post-operative care, etc.), and mask fit/seal issues can complicate therapy, especially in patients with altered consciousness or agitation.
#### **3. Pediatric and Geriatric Patient Care**
Certain patient groups—children, elderly, or those with disabilities—are less able to manage masks themselves or may require gentle, adaptive application.
#### **4. Infectious Disease Control and Isolation Units**
Automation of mask placement in negative-pressure rooms or high-risk environments could reduce healthcare worker exposure.
#### **5. Anesthesia and Sedation**
Precise, automated mask application for sedation or anesthesia could supplement procedures in ORs or outpatient clinics.
#### **6. Rehabilitation Centers and Assisted Living**
In settings where staff-to-patient ratios are low, automating mask delivery could increase therapy availability and quality for users with chronic or progressive conditions.
#### **7. Home Telemedicine and Remote Monitoring**
Integration with telehealth systems to facilitate remote adjustment and monitoring, providing clinicians with more reliable data and enabling virtual check-ins.
—
### **Market Opportunity: Sizing the Need**
#### **A. Sleep Apnea: The Core Market**
**Incidence & Prevalence**
– According to the American Sleep Apnea Association, over 22 million Americans suffer from sleep apnea. Globally, estimates reach 936 million adults aged 30–69 (The Lancet Respiratory Medicine, 2019)—with significant underdiagnosis.
– CPAP/PAP therapy is prescribed to a fraction; in the U.S., about 5–8 million are active PAP users.
**Non-Compliance is Rampant**
– Adherence rates languish between 45-60%. Reasons include mask discomfort, poor fit, skin irritation, and sleep disruption—problems the robotic system directly addresses.
**Market Size – Devices & Accessories**
– The global sleep apnea devices market was valued at $5.9 billion in 2023 (MarketsandMarkets, Grand View Research). The CPAP devices and accessories subsegment makes up ~70% of this market.
– **TAM**: If all OSA-diagnosed patients (assume 100 million globally) and 10% of the suspected undiagnosed population could benefit, the annual device market could exceed $10–15 billion, accounting for devices, masks, and consumables.
– **SAM**: Focusing on U.S. and top 5 EU markets, the early SAM for advanced robotic systems might target the 8–12 million high-risk, non-compliant, or home-ventilated patients—a $3–5 billion wedge, with higher ASP for robotic solutions.
#### **B. Hospital and Critical Care Ventilation**
– The critical care ventilators market (2022) is valued at $1.5 billion globally (Frost & Sullivan, MarketsandMarkets).
– Non-invasive mask ventilation is a significant share, but mask-related complications and nurse labor costs are high.
– Adoption in 10% of U.S./EU hospital beds (over 500,000 beds) at $10,000 per robotic system (capital and service over 4–5 years) yields a market of ~$5 billion.
#### **C. Long-Term and Home Care**
– The U.S. has over 1 million patients on home mechanical ventilation (HME News).
– The “aging in place” trend and rising chronic disease prevalence are expanding demand.
– For the elderly or disabled, a system that reduces dependency and injury risk has strong appeal—estimated long-term/post-acute care TAM $2 billion+.
#### **D. Pediatric and Special Population Needs**
– Children’s hospitals and special care centers for neuromuscular disorders present a niche but high-acuity use case.
– Tens of thousands of children require chronic ventilation or PAP therapy in the U.S.
#### **E. Ancillary Markets**
– Operating rooms and anesthesia have significant, if smaller, potential for procedural automation and workflow optimization.
– Telemedicine and connected health comprise a future growth segment, with increasing demand for remote monitoring, maintenance, and support.
**Summing Across Verticals:**
Combining the above, the **global TAM for robotic automated mask systems** surpasses $15–20 billion, with a SAM (accounting for adoption rates, procurement cycles, and reimbursement realities) of approximately $4–6 billion in the next decade. Early adoption will cluster in high-risk, high-cost, or heavily regulated settings before trickling down to consumer/residential markets.
—
### **Transformative Impact: Solving Barriers to PAP Compliance and Beyond**
#### **Improving PAP Therapy Compliance**
Most sleep professionals agree: the weakest link in OSA therapy is the mask itself. The need for a perfect fit, continual adjustment, and optimal comfort has led to a proliferation of mask shapes, sizes, and materials, but it’s still common for users to abandon therapy. This robotic solution addresses:
– **Personalized, Optimal Fit**: Computer vision tracks facial features in real time, enabling micro-adjustments, minimizing leaks, and maximizing comfort.
– **Timely Application**: Automatically applies mask *after* sleep onset, reducing anxiety or claustrophobia.
– **Adaptive Force Control**: Reduces skin trauma and marks, enhancing comfort for sensitive users.
– **Automated Retraction**: Removes the mask if the user awakens, preventing panic or discomfort.
#### **Healthcare Workforce Efficiency**
In sleep labs, hospitals, and long-term care, mask management is labor-intensive, requiring highly trained staff, frequent patient checks, and manual interventions. Automating these tasks frees up personnel and reduces the risk of infection or exposure (e.g., during COVID-19).
#### **Data and Connected Health**
Continuous integration with biometric and vision systems not only improves physical therapy delivery, but generates extensive therapy data, supporting remote monitoring, AI-based risk assessment, and tailored interventions. Regulatory and reimbursement trends increasingly reward such data-driven, outcome-oriented approaches.
—
### **Challenges and Considerations**
– **Cost and Accessibility**: Initial systems will be more expensive than traditional PAP setups, likely restricting early adoption to hospital, sleep center, or high-risk home users. Over time, economies of scale and iterative design can bring costs down for the consumer market.
– **Safety and Reliability**: Any robotics solution interacting with sleeping or unconscious patients carries inherent safety risks that must be mitigated through stringent fail-safes, user overrides, and regulatory compliance (FDA, CE, etc).
– **Interoperability and User Customization**: The system’s success depends on broad mask compatibility, modular accessory design, and seamless integration with existing PAP or ventilator platforms.
– **User Education and Acceptance**: While the system seeks to reduce barriers, some users may be wary of a “robot” in the bedroom. A winning user experience—quiet, unobtrusive, and customizable—is essential.
—
### **Conclusion: A Paradigm Shift for Respiratory Care**
The disclosed robotic arm system signals a major leap in sleep medicine and mask-based ventilation technology. By automating the most troublesome aspect of PAP therapy—mask placement, fit, and comfort—it has the potential to dramatically improve compliance rates, reduce downstream healthcare costs, and expand access to life-saving therapy for millions.
Far from being confined to sleep apnea, the system’s modular, biometrically driven architecture offers solutions in critical care, home ventilation, geriatrics, pediatrics, and beyond. Its integration with modern telemedicine and connected health trends aligns with the healthcare system’s inexorable pivot to automation, personalization, and remote monitoring.
The invention’s total addressable market stretches into the billions, with near-term serviceable opportunities in sleep labs, hospitals, and high-dependency home care. Widespread adoption will require surmounting cost, safety, and training hurdles—but history suggests that technologies solving such critical, persistent barriers rapidly become industry standards.
As sleep and respiratory care continue their transformation, robotic arm systems for automatic mask placement stand poised to reshape not just how we treat sleep apnea, but how we care for vulnerable patients in every setting, from the ICU to the living room.
—
**About the Author**
[Your Name] is a registered U.S. patent attorney and medical device industry expert. For more in-depth IP strategy analyses or to explore commercialization pathways for advanced medical robotics, contact [Your Practice Name] today.
Click here and search US 20250161619 A1.